Abstract
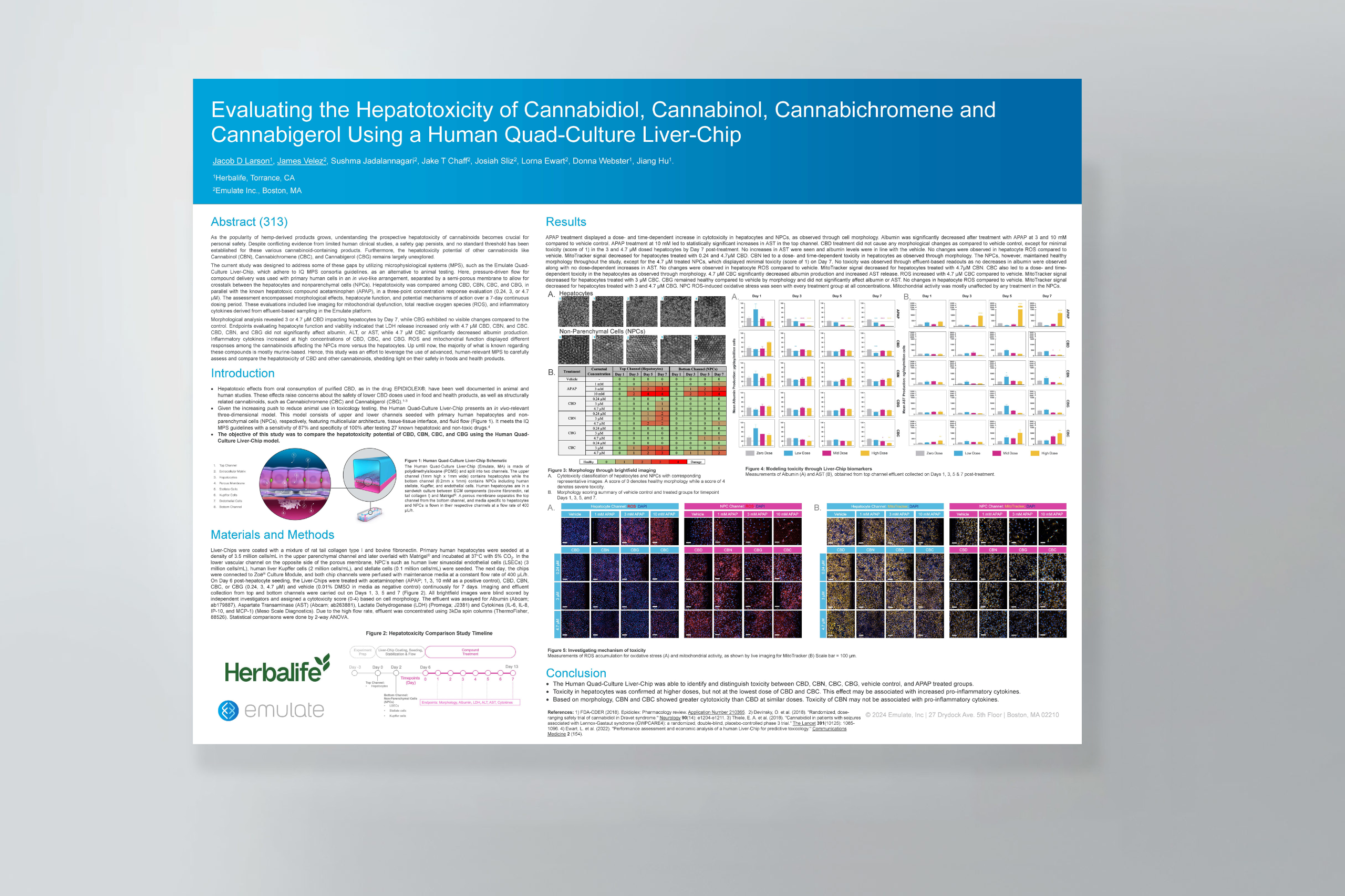
As the popularity of hemp-derived products grows, understanding the prospective hepatotoxicity of cannabinoids becomes crucial for personal safety. Despite conflicting evidence from limited human clinical studies, a safety gap persists, and no standard threshold has been established for these various cannabinoid-containing products. Furthermore, the hepatotoxicity potential of other cannabinoids like Cannabinol (CBN), Cannabichromene (CBC), and Cannabigerol (CBG) remains largely unexplored.
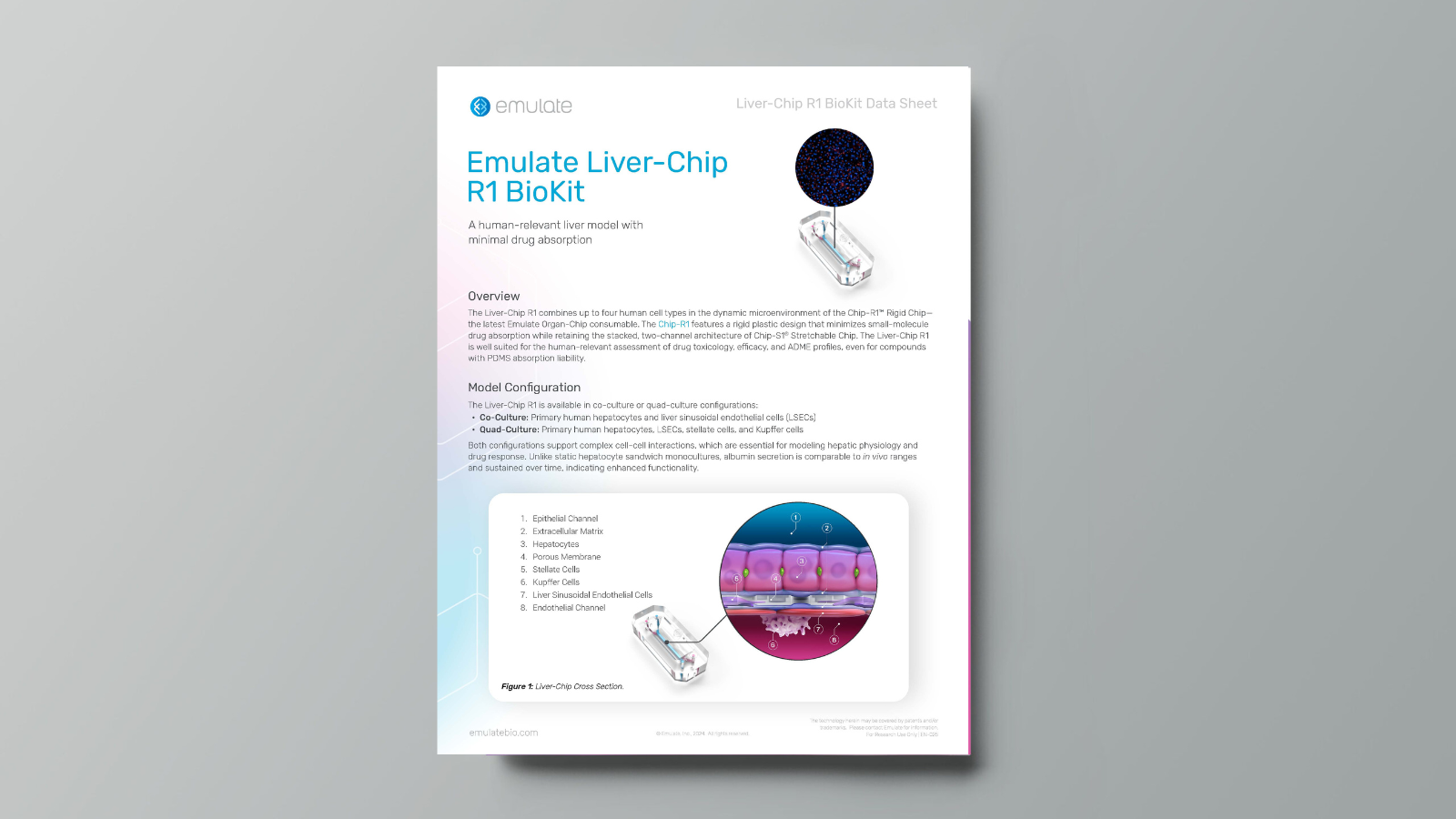
The current study was designed to address some of these gaps by utilizing microphysiological systems (MPS), such as the Emulate Quad-Culture Liver-Chip, which adhere to IQ MPS consortia guidelines, as an alternative to animal testing. Here, pressure-driven flow for compound delivery was used with primary human cells in an in vivo-like arrangement, separated by a semi-porous membrane to allow for crosstalk between the hepatocytes and nonparenchymal cells (NPCs). Hepatotoxicity was compared among CBD, CBN, CBC, and CBG, in parallel with the known hepatotoxic compound acetaminophen (APAP), in a three-point concentration response evaluation (0.24, 3, or 4.7 µM). The assessment encompassed morphological effects, hepatocyte function, and potential mechanisms of action over a 7-day continuous dosing period. These evaluations included live imaging for mitochondrial dysfunction, total reactive oxygen species (ROS), and inflammatory cytokines derived from effluent-based sampling in the Emulate platform.
Morphological analysis revealed 3 or 4.7 µM CBD impacting hepatocytes by Day 7, while CBG exhibited no visible changes compared to the control. Endpoints evaluating hepatocyte function and viability indicated that LDH release increased only with 4.7 µM CBD, CBN, and CBC. CBD, CBN, and CBG did not significantly affect albumin, ALT, or AST, while 4.7 µM CBC significantly decreased albumin production. Inflammatory cytokines increased at high concentrations of CBD, CBC, and CBG. ROS and mitochondrial function displayed different responses among the cannabinoids affecting the NPCs more versus the hepatocytes. Up until now, the majority of what is known regarding these compounds is mostly murine-based. Hence, this study was an effort to leverage the use of advanced, human-relevant MPS to carefully assess and compare the hepatotoxicity of CBD and other cannabinoids, shedding light on their safety in foods and health products.