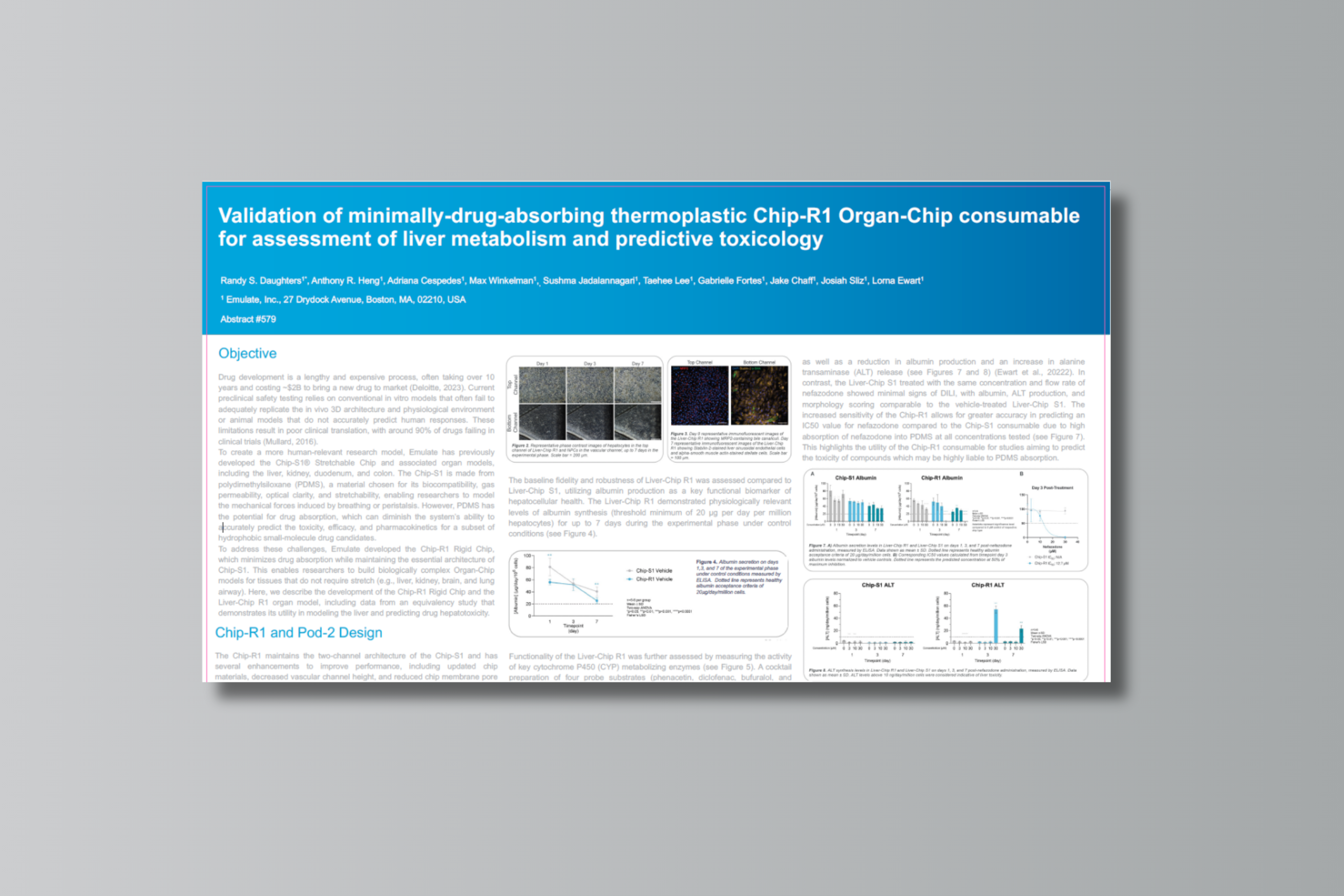
Originally presented at the MPS World Summit 2025 Annual Meeting in Brussels, Belgium.
Authors
Randy S. Daughters1*, Anthony R. Heng1, Adriana Cespedes1, Max Winkelman1, Sushma Jadalannagari1, Taehee Lee1, Gabrielle Fortes1, Jake Chaff1, Josiah Sliz1, Lorna Ewart1
1 Emulate, Inc., 27 Drydock Avenue, Boston, MA, 02210, USA
Abstract
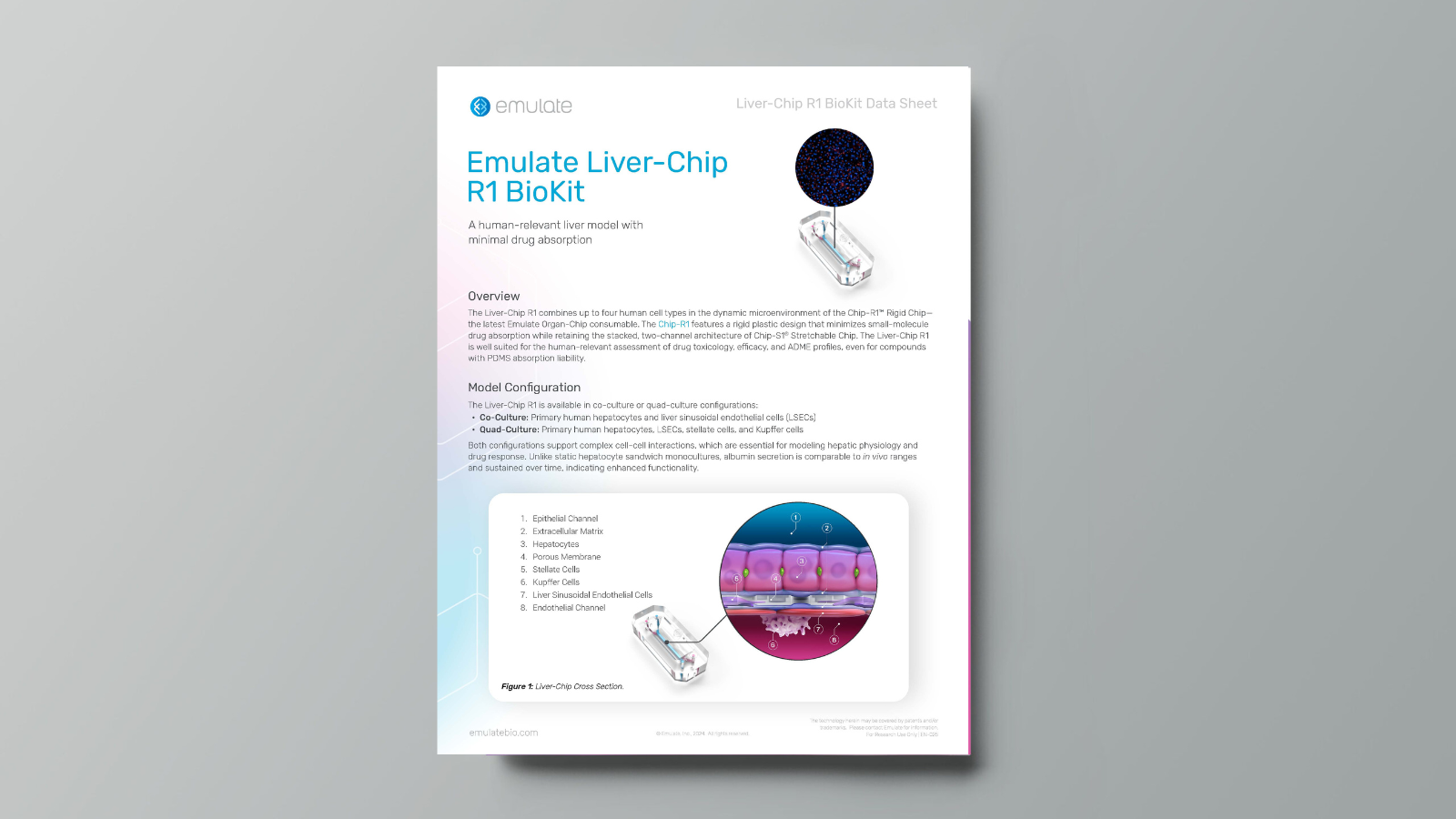
Emulate’s new Chip-R1™ Rigid Chip is a minimally drug-absorbing Organ-Chip consumable designed for improved in vitro toxicology. It incorporates minimally drug absorbing thermoplastics along with a new porous, cell culture-treated membrane that reduce small lipophilic drug absorption. Validated with a quad culture liver model consisting of human primary hepatocytes, liver sinusoidal endothelial cells, Kupffer cells, and stellate cells, Chip-R1 supports physiological features of the liver, including albumin production and small molecule metabolism. Its reduced drug absorption enhances reproducibility and sensitivity in detecting toxicity versus PDMS-based chips. This significant improvement enables more accurate prediction of small molecule toxicity and metabolism in a human-relevant liver model, advancing drug development workflows.