Cancer immunotherapy approaches are having their moment in the clinical spotlight. Over two decades of work characterizing potent activators of the immune system have delivered impressive results with biologic drugs like atezolizumab (Tecentriq) and cell therapies like chimeric antigen receptor T-cell (CAR-T) treatment.
T-cell engaging bispecific antibodies (TCBs) are an emerging class of engineered immunotherapeutic agents that simultaneously bind a cancer cell antigen and the T-cell CD3 receptor. This mechanism activates the T-cell while physically linking it via the target antigen to the cancer cell, which is useful for cells that do not express high levels of immunogenic proteins on their surface or cancers that evade the immune response. As a promising oncotherapy, TCBs are being explored clinically for solid tumor and blood cancers. However, the target antigens are rarely tumor-exclusive; they may be expressed in normal tissues leading to on-target/off-tumor adverse effects that compromise patient safety.
Reliable TCB safety evaluations are critically important to ensuring that immunotherapies are both effective and well-tolerated. The ability to accurately predict therapeutic efficacy and safety remains a challenge. Animal models and two-dimensional (2D) cell culture models of tissues and organs, such as transwells, have been used for the purpose with some success, but are also subject to limitations. Many therapeutic drugs are designed to target human biology, which differs from the biology of animals. 2D cell culture models lack circulation, immune cells, and the proper microenvironment for target expression and immune cell activation. For example, standard in vitro models also do not capture air interfaces or mechanical forces that mimic breathing and peristalsis critical for the functional properties of organ tissues. Animal preclinical models are often not informative for predicting human cancer immunotherapy-mediated adverse events due to lack of cross-reactivity with drugs targeting human-specific epitopes.
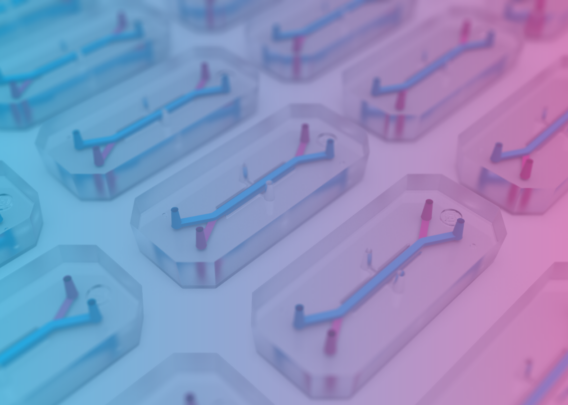
Organs-on-Chips aim to overcome these limitations by modeling the complex multifactorial microenvironment of native tissues and organs and more accurately reflecting the complexity and specificity of human immunity. In a study published in eLife and available on PubMed, researchers from Roche and Emulate assessed in vivo target expression and toxicity of TCBs targeting folate receptor 1 (FOLR1) or carcinoembryonic antigen (CEA) to design and validate Organs-on-Chips as a more human-relevant platform to determine safety and efficacy.
- Research Area: Immunotherapeutic drugs, toxicity testing
- Organisms: human
- Sample Types: human Lung Alveolus-Chip, human Duodenum Intestine-Chip, human Colon Intestine-Chip
- Research Question: Can organs-on-chips be used as human organ models to evaluate the on-target/off-tumor safety and efficacy profiles of TCBs?
Experimental Overview
Lung Toxicity targeting folate receptor-1 (FOLR1)
A TCB to folate receptor-1 (FOLR1), overexpressed in ovarian, lung and breast cancers as well as in normal tissue, was chosen for study of on-target/off-tissue toxicity. This TCB showed high efficacy in human breast tissue xenografts but resulted in severe on-target lung immune toxicity in monkeys.
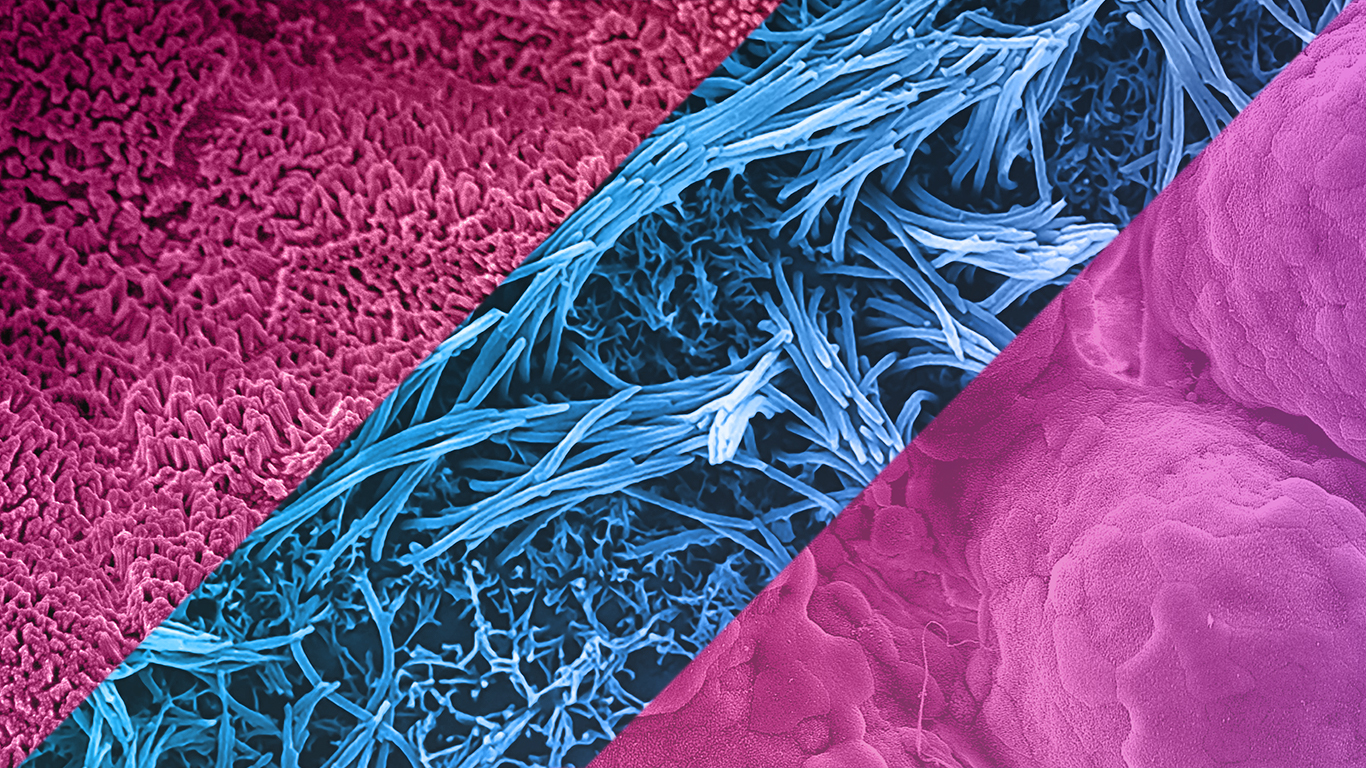
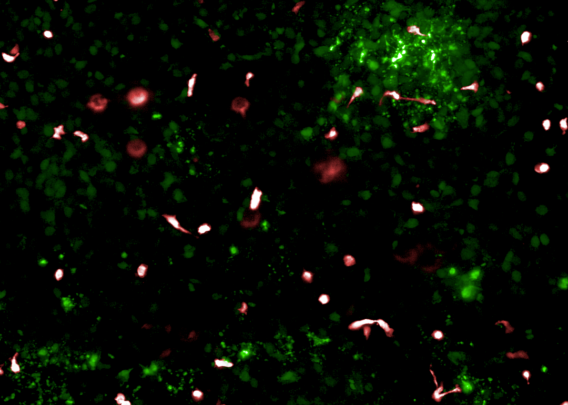
To evaluate the safety of FOLR1 TCBs, an Alveolus Lung-Chip model was developed consisting of primary lung alveolar epithelial cells in the upper chamber exposed to air, with primary microvascular cells established in the lower chamber together with peripheral blood mononuclear cells. Immune activation was measured by T-cell crosslinks to the FOLR1 expressing target cells mediated by the TCB, subsequent T-cell activation, cytotoxic granule release and target cell apoptosis.
In order to determine if cellular immune responses were different depending on the affinity of the antibody for its tumor target, two TCBs with different affinities for the target molecule were tested. FOLR1(hi)-TCB with a high affinity for FOLR1, and FOLR(lo)-TCB with a lower affinity for the same target receptor were examined for cell killing efficacy and for off-target cytotoxicity. The authors found that the lower affinity molecule had a better safety profile than the higher affinity one, which was also recapitulated in a primate animal model. Notably, a transwell culture version of this experimental setup did not accurately reproduce the animal results.
Gastrointestinal toxicity targeting carcinoembryonic antigen (CEA)
Carcinoembryonic antigen (CEA) is a cell surface antigen expressed in varying amounts in the gut and is often overexpressed in colorectal cancers. A second study with CEA-engaging TCBs, which are specific for humans and not cross-reactive with mouse or monkey CEA, was done using Organ-Chips to assess potential intestinal toxicities.
The researchers profiled two types of Organ-Chips (Duodenum-Intestine and Colon-Intestine) both demonstrating tight, polarized epithelial barriers and mature enterocytes to assess the safety of high- and low-affinity CEA TCB variants. The researchers observed physiologically relevant expression of the CEA target within these intestinal models, and assessed immune cell crosslinking to the target antigen, activation and epithelial cell death.
They saw that the Colon Intestine-Chip had higher expression of the CEA target than the Duodenum Intestine-Chip on the cell surfaces. The Colon Intestine-Chip reproduced the distribution and density found in the native tissue, which was not replicated in static transwell culture. Furthermore, the Intestine-Chip predicted CEA-mediated on-target toxicity, the extent of which was governed by antibody affinity and target abundance, with the colon being more liable to damage compared with the duodenum.
The authors also concluded that the high affinity TCB might induce off-tumor toxicity even in tissues with low target expression such as in the small intestine.
Conclusions
Human immunocompetent models of the lung and intestine were created using Emulate’s Organ-on-a-Chip technology, and they were validated for profiling lung and intestine toxicity of engineered TCBs.
- The Alveolus Lung-Chip reproduced FOLR1 TCB-mediated lung toxicity and instructed the design of a lower affinity antibody with a more favorable safety profile, verified in non-human primates.
- The Colon Intestine-Chip models highlighted the safety liabilities of a TCB that targets a human antigen that lacks an animal counterpart. These experiments showed that the Organs-on-Chips could show sensitivity to antibody affinity and show differences in target-dependent toxicities in different regions of the intestine.
The Organs-on-Chip models developed in this study demonstrate clear advantages over traditional in vitro efficacy and safety models. “With functional features of the human immune system, these models represent a promising alternative platform on which to perform immunotherapeutic safety testing, format selection and optimization” said Lauriane Cabon of Roche, a lead author on the study. In the hands of academic and pharmaceutical researchers, Organ-Chips will reduce reliance on animal-based safety assessments, inform antibody format selection, shed light into the mechanistic underpinnings of toxicities, and potentially support identification of new clinical cancer biomarkers.
“Engineered immunotherapies are highly efficacious but have shown significant clinical safety liability sometimes missed in conventional safety profiling. Advanced immunocompetent Organ-Chip models with the ability to predict off-tumor cytotoxicity in multiple affected tissue types could have a real impact on the drugs selected for clinical assessment, reduce the use of animals, and improve patient outcomes” said S. Jordan Kerns, a lead co-author on the study.