Webinar Abstract
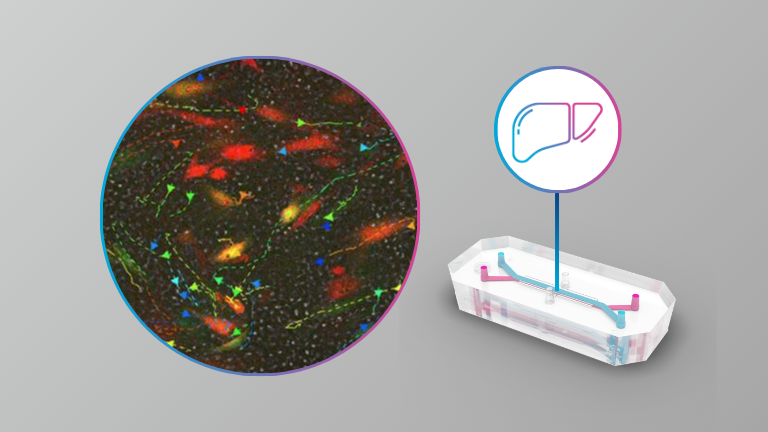
In December 2022, two milestone papers were published: “Predictive validity in drug discovery: what it is, why it matters and how to improve it” in NRDD and “Performance assessment and economic analysis of a human Liver-Chip for predictive toxicology” in Communications Medicine, part of Nature Portfolio. In addition, President Biden signed the FDA Modernization Act 2.0 into law. This groundbreaking advancement allows researchers to leverage Organ-on-a-Chip technology data as part of a novel IND submission, breaking the 1938 Food, Drug, and Cosmetic Act (FDCA) mandate that required all new drugs be tested on animals.
To say the least, it was an exciting way to close out the year. However, these milestones are sparking many questions across the industry: What’s next, how does this impact my work, and how do I get started with Organ-on-a-Chip technology?
Watch this on-demand fireside chat to see industry experts discuss:
- What is predictive validity in drug discovery, why is it important, and how can we improve it?
- The recent Communications Medicine publication demonstrated that the Emulate human Liver-Chip was able to correctly identify 87% of the tested drugs that caused drug-induced liver injury in patients despite passing animal testing evaluations—and did not falsely identify any drugs as toxic, leading to a 100% specificity rating. We will discuss how this will help your decision-making criteria to improve patient safety and increase your confidence that a viable candidate drug will not be de-prioritized due to a false positive.
- How could an improvement in sensitivity and specificity lead to a $3B increase in R&D productivity for small molecule drug development?
- And lastly, what can we expect with the passing of the FDA Modernization Act and the growing global movement to eliminate animal testing mandates?