Abstract
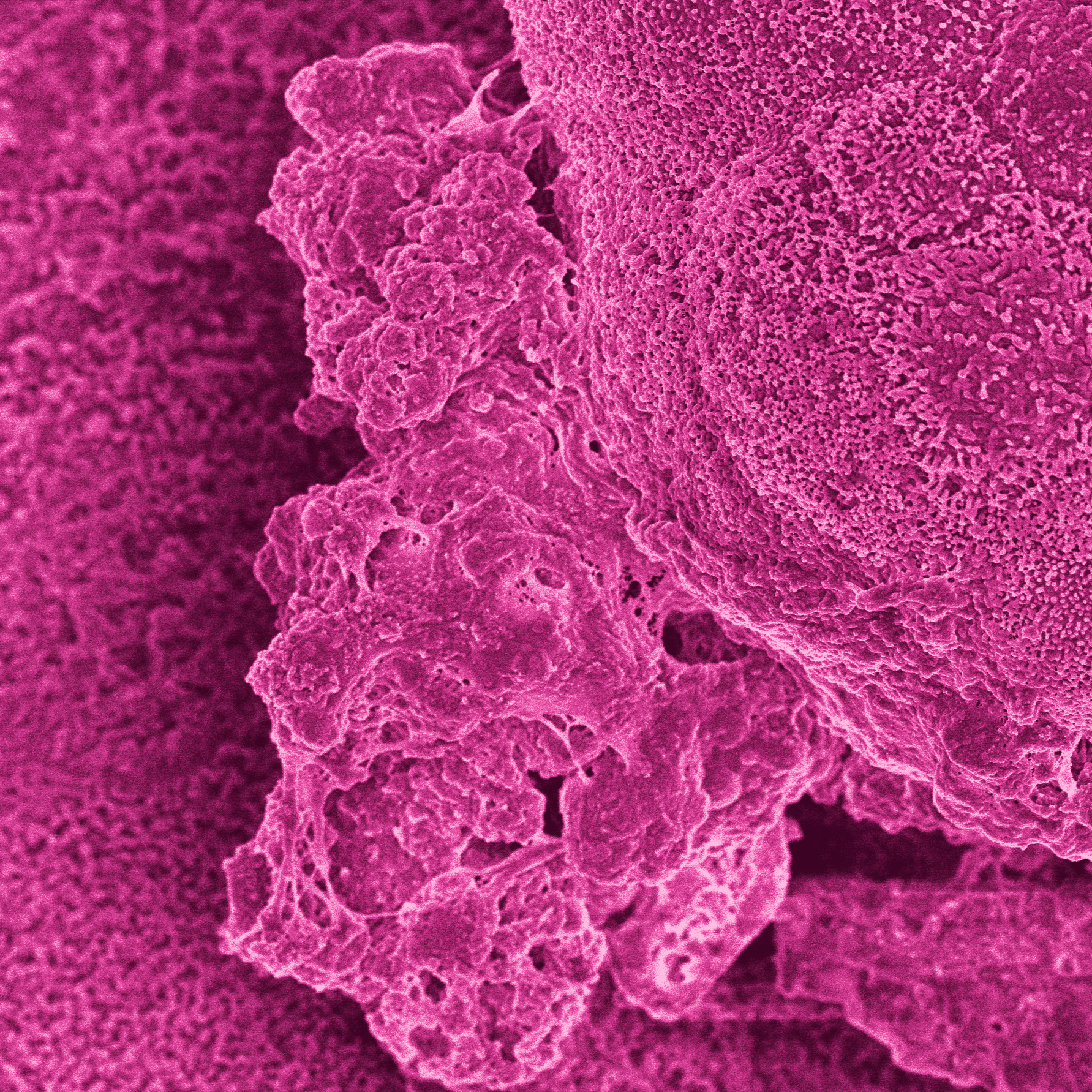
Human milk oligosaccharides (HMOs) shape the gut microbiota in infants by selectively stimulating the growth of bifidobacteria. Here, we investigated the impact of HMOs on adult gut microbiota and gut barrier function using the Simulator of the Human Intestinal Microbial Ecosystem (SHIME®), Caco2 cell lines, and human intestinal gut organoid-on-chips. We showed that fermentation of 2’-O-fucosyllactose (2’FL), lacto-N-neotetraose (LNnT), and combinations thereof (MIX) led to an increase of bifidobacteria, accompanied by an increase of short chain fatty acid (SCFA), in particular butyrate with 2’FL. A significant reduction in paracellular permeability of FITC-dextran probe was observed using Caco2 cell monolayers with fermented 2’FL and MIX, which was accompanied by an increase in claudin-8 gene expression as shown by qPCR, and a reduction in IL-6 as determined by multiplex ELISA. Using gut-on-chips generated from human organoids derived from proximal, transverse, and distal colon biopsies (Colon Intestine-Chips), we showed that claudin-5 was significantly upregulated across all three gut-on-chips following treatment with fermented 2’FL under microfluidic conditions. Taken together, these data show that, in addition to their bifidogenic activity, HMOs have the capacity to modulate immune function and the gut barrier, supporting the potential of HMOs to provide health benefits in adults.