Webinar Abstract
Featured session at Boston MPS Day, which took place on November 1, 2023.
Dr. Saumya Das from Massachusetts General Hospital (MGH) discusses using Organ-on-a-Chip platforms to study how extracellular vesicles (EVs) influence functional biology and disease mechanisms, particularly in cardiometabolic contexts. EVs, including exosomes and other small vesicles, are significant mediators of intercellular communication, carrying microRNAs, proteins, and other cargo that can alter recipient cell behavior. However, understanding their organ-specific effects in humans has been challenging due to limited animal models and difficulties in isolating human tissues under well-controlled conditions.
Leveraging Emulate’s Human Emulation System, Dr. Das’s team focuses on modeling complex human pathologies involving multiple organs, including the kidney, liver, heart, and potentially the brain. He highlights four case studies:
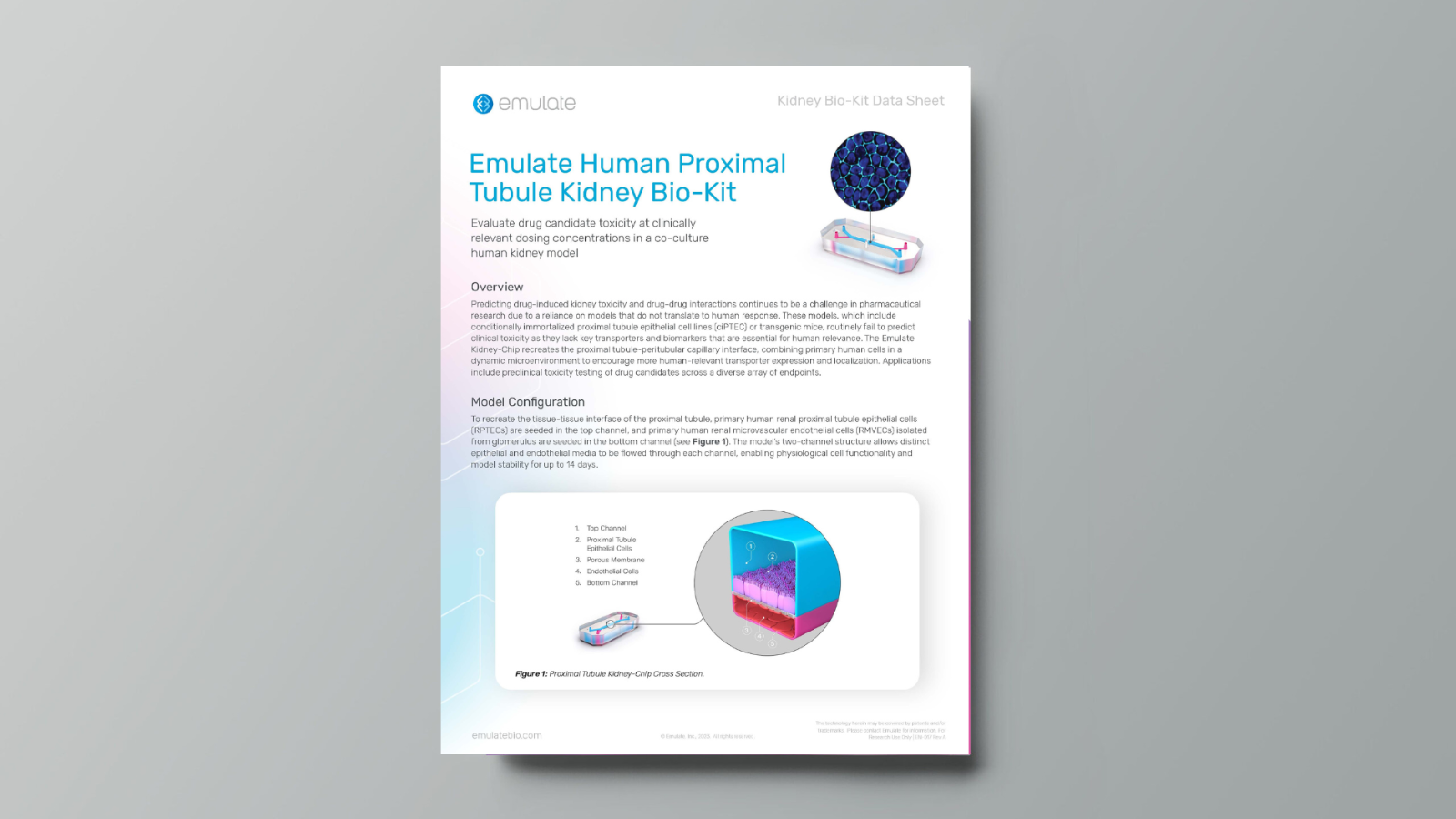
- Cardiorenal Syndrome (Kidney-Chip):
Cardiorenal syndrome involves kidney injury triggered by heart failure and volume overload. Dr. Das’s lab isolated patient-derived EVs and perfused them through the Emulate Kidney-Chip (proximal tubule epithelium and endothelial channels). EVs from patients with cardiorenal syndrome induced significant renal injury markers compared to EVs from heart failure patients without renal involvement or from healthy controls. Through multi-omics analyses (particularly microRNA profiling), they identified EV-contained microRNAs that modulate TGF-β signaling and drive kidney injury. Inhibition experiments confirmed that these microRNAs were both necessary and sufficient to replicate the disease phenotype, offering new mechanistic insights and potential therapeutic targets.
- Obesity-Related Liver Disease (Liver-Chip):
Obesity-derived EVs (notably from adipose tissue) were introduced into a Liver-Chip model. By creating a non-alcoholic fatty liver disease (NAFLD)-like environment and adding adipose-derived EVs, they observed lipid droplet accumulation and transcriptomic changes reminiscent of NAFLD. This platform allows for in-depth study of how EVs from obese patients affect hepatic metabolism and gene expression, potentially guiding future treatments for metabolic liver diseases.
- Organ Crosstalk via EVs:
Dr. Das’s lab extended their Liver-Chip studies to investigate EV release dynamics and their effects on other organs. For instance, EVs secreted under NAFLD conditions can be introduced to human cardiomyocytes or other tissue chips (e.g., neural tissues) to dissect mechanisms of systemic metabolic and inflammatory signals.
- Future Brain-Chip Studies:
Planned investigations will explore neuroinflammation and obesity-related brain changes with a Brain-on-a-Chip model. The team aims to understand if EVs derived from diseased tissues (e.g., adipose or liver) contribute to neuroinflammation and cognitive dysfunctions.
Key learnings from this presentation include:
- Human-relevant EV studies: MPS models provide a controlled, species-matched environment to study patient-derived EVs without the confounding factors of animal models.
- Mechanistic insights: Using multi-omics and gene perturbation experiments on Kidney or Liver-Chips revealed critical microRNA-driven pathways (e.g., TGF-β in cardiorenal syndrome), illuminating novel disease mechanisms and potential intervention points.
- Complex disease modeling: Combining EV treatments with disease-specific conditions (e.g., heart failure, NAFLD) on chips simulates human organ crosstalk and systemic pathophysiology, allowing exploration of how EVs contribute to multi-organ disorders.
- Personalized and translational research: With patient-derived EVs and chips modeling key human organs, researchers can identify actionable targets and biomarkers, bridging fundamental biology with clinical implications for complex cardiometabolic diseases.