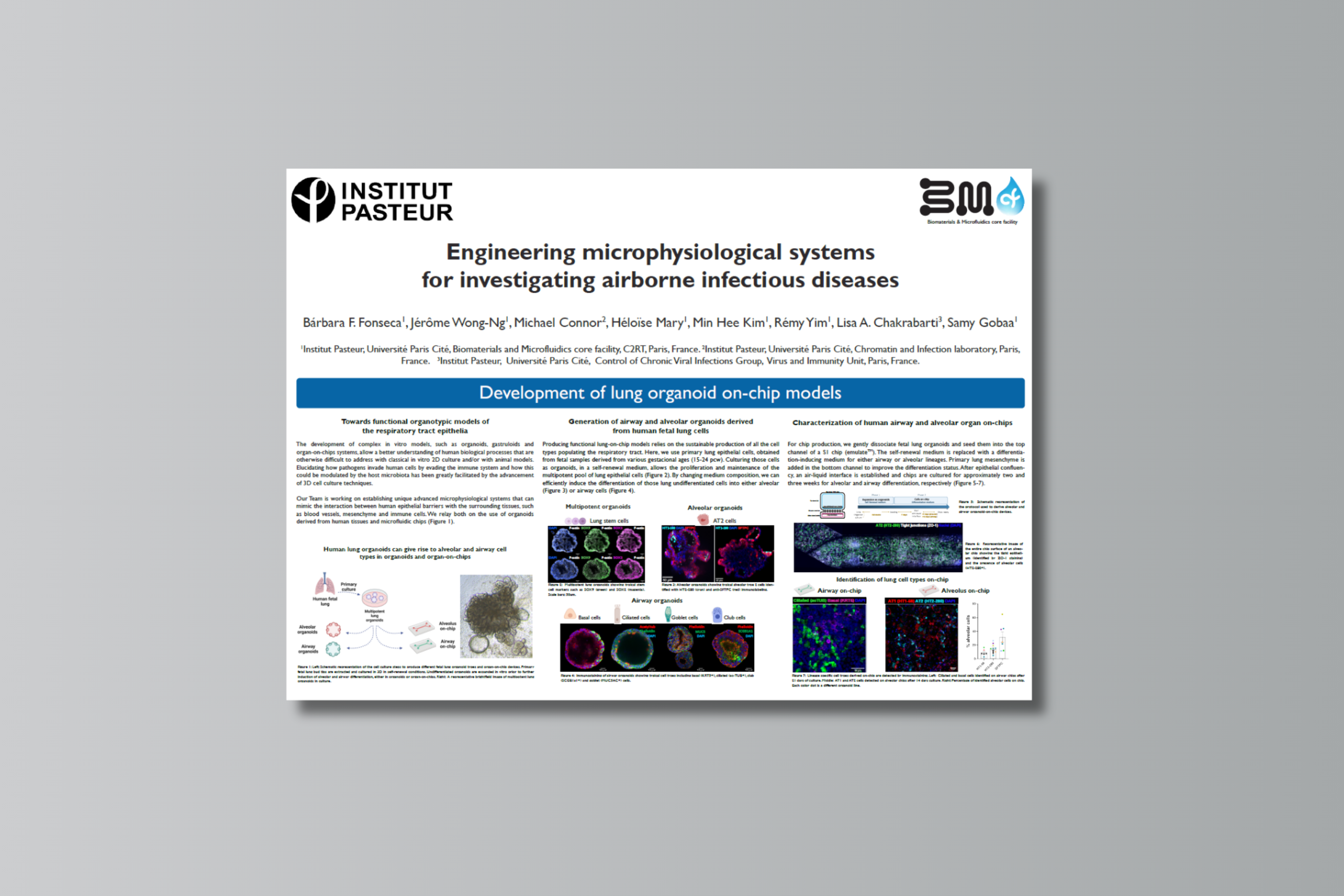
Originally presented at the MPS World Summit 2025 Annual Meeting in Brussels, Belgium.
Authors
Bárbara F. Fonseca1, Jérôme Wong-Ng1, Michael Connor2, Héloïse Mary1, Min Hee Kim1, Rémy Yim1, Lisa A. Chakrabarti3, Samy Gobaa1
1Institut Pasteur, Université Paris Cité, Biomaterials and Microfluidics core facility, C2RT, Paris, France. 2Institut Pasteur, Université Paris Cité, Chromatin and Infection Laboratory, Paris, France. 3Institut Pasteur, Université Paris Cité, Control of Chronic Viral Infections Group, Virus and Immunity Unit, Paris, France.
Abstract
The development of complex in vitro models, such as organoids, gastruloids and organ-on-chips systems, allow a better understanding of human biological processes that are otherwise difficult to address with classical in vitro 2D culture and/or with animal models. Elucidating how pathogens invade human cells by evading the immune system and how this could be modulated by the host microbiota has been greatly facilitated by the advancement of 3D cell culture techniques. Our Team is working on establishing unique advanced microphysiological systems that can mimic the interaction between human epithelial barriers with the surrounding tissues, such as blood vessels, mesenchyme and immune cells. We relay both on the use of organoids derived from human tissues and microfluidic chips.