Historical Roots of Mandated Animal Testing
Animal use in U.S. biomedical research has been both guided and constrained by laws that date back to the 1938 Food, Drug & Cosmetic Act, which effectively required animal data before human trials could begin. Yet almost as soon as that mandate was in place, pressure to curb its excesses arose. In 1959, British scientists William Russell and Rex Burch articulated the now-canonical “3 Rs” (Replace, Reduce, Refine) in The Principles of Humane Experimental Technique, giving regulators and ethicists a common language for alternatives1.
Through the 1970s and 1980s, advocacy groups such as the Humane Society of the United States, the Physicians Committee for Responsible Medicine, and later PETA turned laboratory animal welfare into a mainstream public concern. Their campaigns helped secure passage of amendments to the U.S. Animal Welfare Act and spurred the first congressional hearings on alternatives to animal testing in drug development.
The scientific establishment followed. In 1997, eleven federal agencies formed the Interagency Coordinating Committee on the Validation of Alternative Methods (ICCVAM), and Congress cemented its role with the ICCVAM Authorization Act of 2000. ICCVAM’s charter is explicit: accelerate regulatory acceptance of test methods that replace, reduce, or refine animal use without compromising safety or efficacy2.
Momentum grew when the National Research Council’s 2007 report, “Toxicity Testing in the 21st Century,” urged a wholesale shift toward human-relevant, high-throughput assays and computational models3. That vision seeded collaborative programs like Tox21, an EPA-, NIH-, and FDA-backed effort that screens thousands of chemicals in robotics-driven, cell-based platforms instead of rodents4. Across the Atlantic, the European Union’s phased-in ban on animal-tested cosmetics—culminating in a full marketing ban in 2013—proved that large markets could operate under strict animal-free requirements without stalling innovation5.
Why This Marks an Inflection Point
Despite this steady drumbeat, U.S. federal drug-development rules remained largely unchanged—until recently. Over the past 3 years, and especially within the last twelve months, a cascade of legislative and agency actions has transformed decades of advocacy into concrete policy. What once felt aspirational is now operational: sponsors are no longer merely allowed to submit New Approach Methodologies (NAMs); they are increasingly expected to do so. That rapid acceleration marks 2024-2025 as an unmistakable inflection point: one in which scientific maturity, public pressure, and regulatory authority have finally aligned to make human-relevant models the new default for preclinical research.
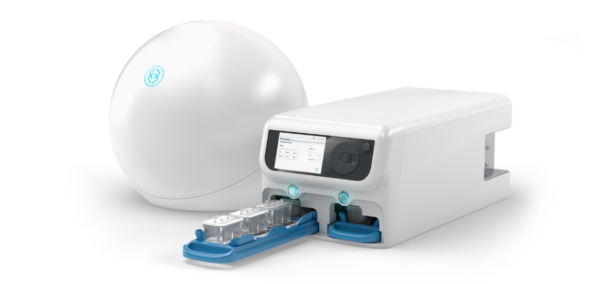
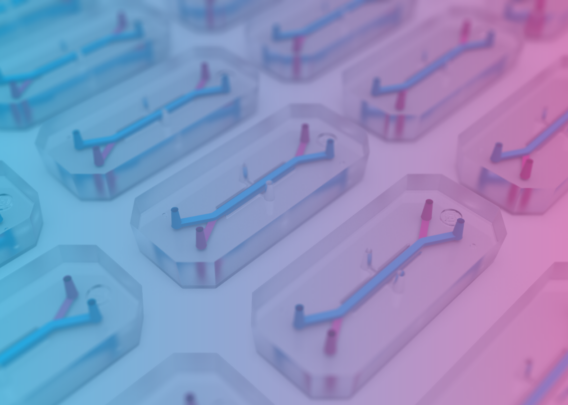
Over the past three years, the United States has moved from discussion to implementation in modernizing drug-development rules that were once completely reliant on animal testing. Catalyzed by bipartisan legislation, agency-specific pilot programs such as FDA’s ISTAND program, and mounting scientific validation of New Approach Methodologies (NAMs) such as Organ-on-a-Chip technology, a clear through-line has emerged: regulators now expect—and increasingly require—human-relevant tools to inform safety and efficacy in preclinical research. Below is a chronological look at the key milestones, followed by a recap of how Emulate has helped drive and shape this historic shift.
Recent Timeline of Policy Milestones
DATE | AGENCY | MILESTONE & IMPACT |
Dec 2020 | FDA | ISTAND Program Launch. Opens formal pathway for novel Drug Development Tools such as Organ‑Chips. |
Dec 29, 2022 | US Congress | FDA Modernization Act 2.0. Removes statutory animal‑test mandate; defines “nonclinical tests” to include in vitro, in silico and microphysiological systems. |
Feb 6, 2024 | US Congress | FDA Modernization Act 3.0 (introduced). Directs FDA to build a routine qualification pathway for NAMs. |
Sep 24, 2024 | FDA | First Organ‑Chip accepted into ISTAND. Emulate's submission of the Liver‑Chip S1 for predicting DILI establishes evidentiary precedent. |
Apr 10, 2025 | FDA | Roadmap & Phase‑Out Plan. Animal studies to become “the exception”; prioritizes MPS data and AI‑driven models. |
Apr 29, 2025 | NIH | Funding Priorities Shift. Grants now favor human‑based technologies over animal‑only studies. |
May 29, 2025 | US Navy | Ends Cat & Dog Experiments. Signals wider federal move toward NAMs. |
Jul 7, 2025 | NIH | Bars Animal‑Only Proposals. Requires at least one validated human‑relevant method in funded research. |
December 2020 — FDA launches ISTAND Program
Recognizing the need to facilitate the approval of beneficial technologies for drug development that fall outside the scope of existing Drug Development Tool (DDT) qualification programs, in late 2020, the FDA introduced the Innovative Science and Technology Approaches for New Drugs (ISTAND) Program. In their explanation of the ISTAND program, the FDA explicitly listed microphysiological systems such as Organ-Chips as an example technology that would qualify for entry into the program. Ultimately, technologies approved for a context of use through the ISTAND program can be included in IND and NDA applications “without needing FDA to reconsider and reconfirm its suitability.”6
December 29, 2022 — FDA Modernization Act 2.0 becomes law
Congress eliminated the Depression-era mandate that animal data be the default gateway to human trials, explicitly authorizing cell-based assays, microphysiological systems (MPS), and sophisticated computer models as equally valid evidence. The amending language accomplishing this was quite simple: the new act removed the phrase “preclinical tests (including tests on animals)” from the original law, and replaced it with “nonclinical tests”. Nonclinical test were further defined as “…a test conducted in vitro, in silico, or in chemico, or a non-human in vivo test that occurs before or during the clinical trial phase of the investigation of the safety and effectiveness of a drug, and may include animal tests, or non-animal or human biology-based test methods, such as cell-based assays, microphysiological systems, or bioprinted or computer models.”
While the changes to the original law were simple, their effects were profound. The statute not only empowers sponsors to use NAMs, it also instructs FDA reviewers to consider them on their scientific merits7,8.
February 6, 2024 — FDA Modernization Act 3.0 introduced
Building on the 2022 breakthrough, the 3.0 bill directs the FDA to create a formal pathway for the qualification, review, and routine acceptance of non-animal methods. If enacted, it would put the agency on a clock to translate legal authority into day-to-day regulatory practice, closing any remaining gaps that slow the adoption of NAMs9.
September 24, 2024 — First Organ-on-a-Chip admitted to FDA’s ISTAND Pilot Program
FDA’s ISTAND initiative, created to qualify novel Drug Development Tools, accepted the first Organ-on-a-Chip submission: a liver MPS designed to predict drug-induced liver injury (DILI). This seminal acceptance signaled that complex microfluidic models can progress through the same evidentiary pipeline as traditional models10.
April 10, 2025 — FDA announces phased elimination of routine animal testing & releases Roadmap
In a pair of same-day actions, the agency published:
- A policy plan to “reduce, refine, and ultimately replace” animal studies, prioritizing MPS data and AI-driven toxicity modeling in Investigational New Drug (IND) submissions.
- A detailed Roadmap that lays out short-, mid-, and long-term steps—validation standards, cross-agency collaborations, and pilot incentives—to mainstream NAMs across all Centers.
Taken together, the documents move the conversation from permission to expectation, stating that animal use should become “the exception rather than the rule.”11,12
April 29, 2025 — NIH shifts funding priorities toward human-based technologies
America’s largest source of funding for biomedical research launched an initiative to prioritize grant applications that incorporate Organ-Chips, organoids, or computational models—an early indication that future paylines will reward researchers who leave “animal-only” study designs behind13.
May 29, 2025 — U.S. Navy ends cat and dog experiments
The Department of the Navy formally stopped all biomedical research on companion animals, citing the availability of advanced human-based platforms and ethical stewardship of federal resources. Although limited in scope, the decision adds military pressure to the broader federal trend away from animal models14.
July 7, 2025 — NIH bars funding for animal-only studies
Just nine weeks after its technology push, the NIH announced that proposals relying exclusively on animal data will no longer be eligible for agency support. Investigators must integrate at least one validated human-relevant method, accelerating the scientific community’s pivot toward NAMs15.
Emulate’s Contributions to the Sea Change
1. Giving NAMs a Voice on Capitol Hill
Before Congress voted on the FDA Modernization Act 2.0, Emulate submitted formal testimony underscoring how Organ-on-a-Chip technology can improve translational accuracy while reducing animal use. The company’s perspective helped lawmakers grasp the real-world readiness of NAMs and the economic upside of faster, failure-proof pipelines16.
2. Generating the Evidence Base
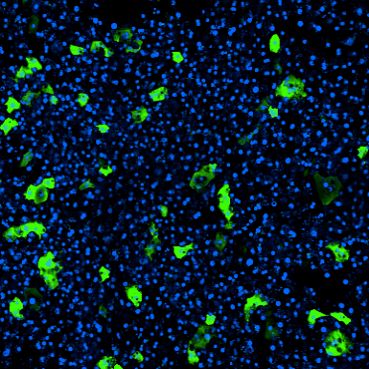
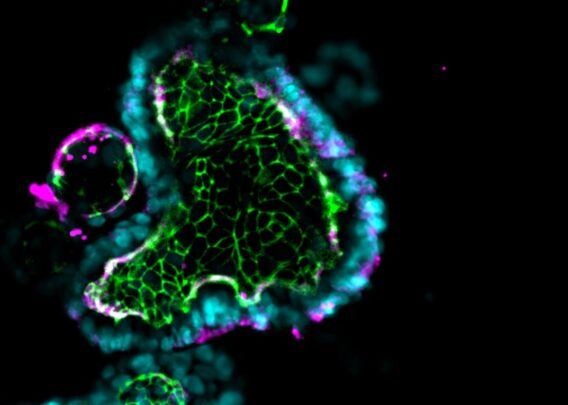
In the largest head-to-head study of its kind, Emulate’s peer-reviewed Nature publication demonstrated that the human Liver-Chip S1 outperforms animal models for predicting DILI, showing 87% sensitivity and 100% specificity for a set of hepatotoxic drugs that animal models had deemed safe. Those data have since been cited by regulators and pharma R&D teams alike as proof that chips can surpass conventional in vivo benchmarks17,18.
3. Achieving the First-Ever ISTAND Acceptance
The Emulate Liver-Chip S1 became the first Organ-Chip welcomed into FDA’s ISTAND Program—setting a procedural precedent for all future MPS tools. Emulate’s submission not only opened the door for chip qualification; it provided the cross-disciplinary dossier that FDA reviewers will use as a template19,20.
4. Being the Only Organ-Chip Manufacturer Cited in FDA’s Roadmap
When FDA mapped its strategy to cut animal testing, it highlighted Organ-Chips—specifically referencing Emulate’s platforms—as validated NAMs ready for wider deployment. That acknowledgment elevated the technology from promising to actionable in the eyes of regulators, funders, and biopharma stakeholders21,22.
5. Convening Thought Leaders Around the New Rules
Shortly after the Roadmap’s release, Emulate hosted a fireside chat with FDA Senior Advisor Dr. Tracy Beth Høeg, Wyss Institute founder Dr. Don Ingber, and Moderna scientist Dr. Samantha Atkins to unpack what the policy means for sponsors. The session offered pragmatic guidance on designing IND packages that lean heavily on human-relevant data—effectively turning policy into a playbook23,24.
Looking Ahead
From Congress to the lab bench, momentum now aligns toward a future where Organ-on-a-Chip technology, advanced in silico models, and other NAMs form the backbone of drug safety assessment. Through our early advocacy, scientific rigor, and collaborative posture, Emulate is proud to have played a role in shifting the regulatory tides. As agencies implement their roadmaps and funders enforce new criteria, technologies that accurately recapitulate human biology will become indispensable. The era of relying on animal proxies is closing; what follows is a more predictive, ethical, and efficient research ecosystem—one that Emulate is excited to be a part of!
Ready to future-proof your pipeline?
Explore our portfolio of sophisticated and user-friendly platforms that make it easy to get started with Organ-on-a-Chip technology.