A summary of the scientific paper published in Advanced Science, “Is it Time for Reviewer 3 to Request Human Organ Chip Experiments Instead of Animal Validation Studies?“
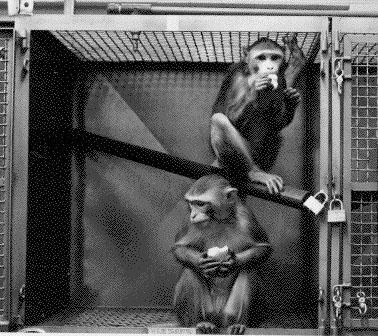
Animal studies are an old practice, going back to the ancient Greeks, continuing with William Harvey and others in the 16th and 17th centuries and gaining greater traction in the past 100 years. Animal models offer more complexity than simple cell cultures, though they fall short of human physiology. But even with their known shortcomings, animal studies have been the gold standard for preclinical research – until now.
To a large degree, the preference for animal studies was by necessity. Preclinical animal models were the best available research tools. However, in recent years, microfluidic Organ-Chips and other technologies have begun to offer superior alternatives. Because they use human tissues – in some cases cultured from patients – they can more accurately recapitulate many of the mechanisms associated with human physiology and bring us closer to personalized medicine.
As many as 90% of all drugs that enter human clinical trials fail to gain FDA approval. Sometimes they are not effective and often, they are just too toxic. Our preclinical models should be able to catch these deficits before the drugs reach patients. However, the current system produces human suffering and wastes valuable time – we must identify better approaches.
THE PROMISE OF ORGAN-CHIPS
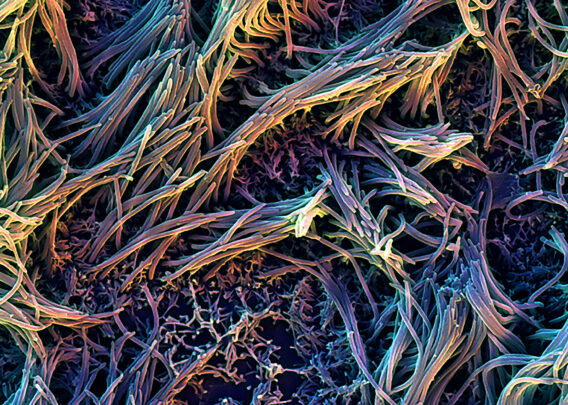
Microfluidic Organ-Chips offer a superior model because they can be built with human tissues and incorporate key physiological components, such as a vasculature, tissue-tissue interfaces, circulating immune cells, and even a complex microbiome. Mechanical forces, such as those associated with breathing or peristalsis, can be replicated as well. Advanced fluidics bring in nutrients, remove waste, and permit mimicry of dynamic changes in drug levels over time, better recapitulating what patients experience in vivo.
These chips are transparent and small, which means researchers can observe reactions continuously, in real time, through microscopes or more advanced systems – something that cannot be done in animal models.
But most importantly, from a drug development standpoint, these chips have been proven to provide important windows into human physiology and provide greater insight into how specific cells and tissues respond to therapeutic molecules. For example, lung chips have replicated human COPD and non-small cell lung cancer. Organ-chips have also modeled intestines, blood-brain barrier, bone marrow, liver, kidneys and numerous other organs and tissues.
Organ-Chips can be particularly useful when investigating human immune responses. Different species of mammals have different immune systems, which can make them ineffective models when studying vaccines, cancer immunotherapies or autoimmune disease treatments.
One chip, modeling a single organ system, can be quite powerful. But these devices also can be linked fluidically for multi-organ studies, creating even more sophisticated “body-on-chips” models. These systems can incorporate many of the complex inter-organ signaling mechanisms found in the human body – for example, pancreatic islet cells can talk to liver tissue. Investigators can even model many of the complexities associated with the reproductive system.
THE COST OF FAILURE
The computer industry has a saying – garbage in, garbage out – and that could easily be applied to the biopharmaceuticals drug development pipeline. Inadequate preclinical models translate into failed drugs. If this were a purely academic discussion, the industry could be forgiven for moving slowly. But these poor models have real world ramifications when ineffective and/or toxic drugs enter human trials where at best they fail to deliver hoped-for benefits or worse, cause patients physical harm.
Organ-Chips have proven themselves over and over, identifying toxicities that went previously undetected in animal studies but unfortunately showed up in human trials. In one instance, a Blood Vessel-Chip retrospectively revealed the faults in a monoclonal antibody therapy that led to blood clot formation in the lung. Unfortunately, the drug had already caused deaths in the human study.
Better preclinical reads on efficacy and safety mean drugs that would have been likely to fail in human trials can be shelved or redesigned. Medicines that work best in subpopulations can be tested early in those populations, rather than failing in a large trial and being reapplied to the smaller group as a consolation prize. Ultimately, making the system more efficient could accelerate our ability to conduct successful clinical trials, dramatically reducing costs and bringing new therapies to patients faster.
But it’s not just about drugs that show promise in animal models and fail in humans. We must also assume there are molecules that fail in animals but are safe and effective in people. However, we approach this problem, it’s obvious we are leaving good drugs on the table.
This is not to say that Organ-Chips are perfect models. They have trouble replicating peripheral neurons, fat and other tissues, which could generate serious blind spots. More work needs to be done to help these emerging research tools better incorporate in vivo human physiology. And that’s really the point. We can no longer be satisfied with the flawed preclinical models that have produced such poor results. Under the current regime, unmet medical needs, such as Alzheimer’s disease, continue to be unmet, and patients, caregivers and communities suffer. Microfluidic Organ-Chips will not solve all these issues, but they will provide insights animal models do not and will ultimately bring a more rational approach to our preclinical discovery efforts.