In this Emulate guest blog, Vivek Thacker, PhD, Group Leader at University Hospital Heidelberg, explains how he and his team at his previous organization, École Polytechnique Fédérale de Lausanne, used the Emulate Lung-Chip to study how bacterial “cords” contribute to the pathogenesis of Mycobacterium tuberculosis.
What is tuberculosis, and what makes it so interesting to study?
Tuberculosis (TB), an infectious bacterial disease, is humankind’s oldest and deadliest foe, still responsible for roughly 1.5 million deaths per year globally. The causative bacterium, Mycobacterium tuberculosis (Mtb), has co-evolved with humans over thousands of years, making TB a chronic disease with a wide spectrum of manifestations. Today, the most common treatment is a multi-drug antibiotic regimen that needs to be administered for several months, leading to poor treatment compliance and an increasing profile of drug resistance.
Interestingly, many individuals in high-risk countries are frequently exposed to Mtb but do not go on to develop TB or adaptive immune responses to Mtb antigens. This suggests that it is important to understand how the human innate immune system effectively halts disease progression. As such, my team and I wanted to characterize Mtb’s earliest interactions with epithelial cells and macrophages in the lung, study how Mtb adapts to the lung microenvironment, and investigate what causes tissue resident immune cells to succeed or fail in their quest to contain infection.
What makes tuberculosis so challenging to study?
TB is spread by aerosols, meaning that the earliest host-pathogen interactions should be single-cell interactions in the vast alveolar spaces of the lung. However, early TB activity in these alveolar spaces is relatively understudied, as it is difficult to isolate a few hundred bacteria in the lungs of any animal model, and it is even more challenging to study the spatiotemporal dynamics of host-pathogen interactions, particularly in BSL-3 conditions.
How did Organ-Chips allow you to overcome these challenges?
These challenges are perfectly suited to Organ-Chips, which fit into the large space in the “middle”—that is, they recapitulate complex cellular interactions that do not occur in simple model systems, allowing us to study the mechanisms of early-stage bacterial exposure and response with high spatiotemporal resolution. As you can imagine, this opens many new research avenues.
Organ-Chips are invaluable for discovery research, allowing us to identify new phenomena or roles for certain cell types in specific host niches. On top of this, the modular nature of this technology allows us to perturb only specific cells in a co-culture for targeted studies. Many “traditional” assays can also be made more precise and quantitative—e.g., fast and accurate measurements of bacterial killing and regrowth after antibiotic treatment. Organ-Chips also enable new kinds of measurements, such as in situ electron microscopy.
Can you describe the model you developed and the insights it yielded?
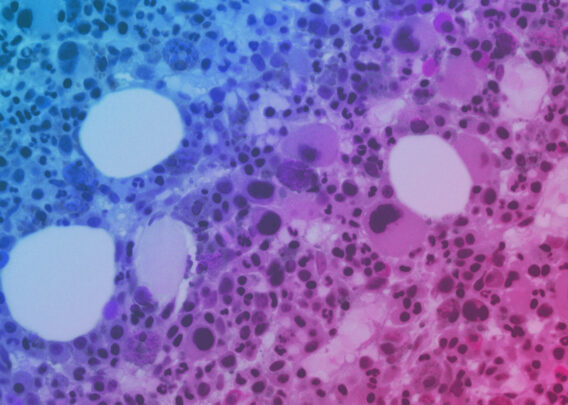
The Lung-Chip recreates the physiological air-liquid interface seen in alveolar biology while being accessible to long-term live-cell imaging. Using this model, we found that pulmonary surfactant secreted by epithelial cells protected the host from Mtb infection, rendering many Mtb unable to grow in host cells. However, exposure to surfactant in turn stimulated the bacteria to produce lipids that survived this first interaction, leading to the formation of biofilm-like cords in host cells that help Mtb bacteria evade clearance by antibiotics.
The consistent growth of Mtb cords in the Lung-Chip led us to search for these structures in the early stages of infection. To do this, we designed an experimental strategy wherein we imaged thick tissue slices with confocal microscopy in order to search for these cords in situ. We were then able to identify cords in an animal model, not only providing crucial validation but also expanding the predictive reach of the Organ-Chips. This provides a roadmap for future iterative development of the Lung-Chip to explore more aspects of Mtb pathogenesis.
How have these findings changed your research, and what does the future look like for you?
Clearly demonstrating that cords play a role in Mtb pathogenesis opens several new research avenues. In future studies, we will seek to understand how the mechanical rigidity of these structures affects immune function as well as focus on dissecting this complex host-pathogen interaction, with the aim to develop better protective strategies. We will also focus on gaining a better understanding of antibiotic responses within specific tissue microenvironments. Using Organ-Chips, we can study how specific tissue niches and barriers change the “effective” antibiotic concentrations that bacteria may experience and how these antibiotics may be processed differently within these bacteria (e.g., restricted access due to tight packing in cords).
Learn more in the full article published in Cell.